- Department

Overview
Contact us
- Research
Research in brief
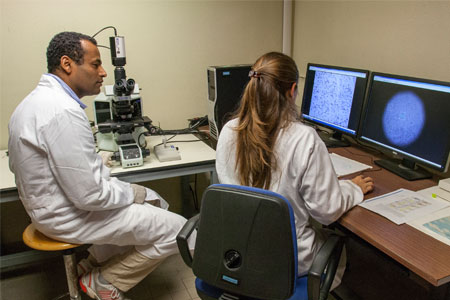
Research activities
Research Facilities
- Teaching

PhD programmes and postgraduate training
Teaching services
- Community Engagement

Information for community
Contact us
- People
- contacts
-